Novel SOI-Biosensor Topology for the Detection of an Acute Myocardial Infarction Marker — Troponin I
A biosensor based on field-effect transistors on silicon-on-insulator structures (SOI-biosensor) is a high-potential device for detection of biological molecules, for instance, such as troponin I; the biosensor allows conducting label-free real-time analysis.
The aim of the study is the development of SOI-biosensor design for detection of acute myocardial infarction marker — troponin I.
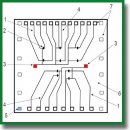
A notable feature of this design was the integration of two grounding electrodes directly onto the biosensor surface, which effectively nullified the static potential of the liquid sample and minimized physical breakdowns of biosensor elements.
Materials and Methods. The highly specific anti-troponin I DNA aptamer was used as a receptor for specific detection of protein marker. Aptamer immobilization on the biosensor surface was carried out by physical adsorption. The analyzed range of target troponin I molecules concentration in the sample varied within 10–11 to 10–9 mol/L, mirroring clinical levels observed in myocardial infarction cases. During the experiment, a constant voltage of Vds=0.15 V was maintained.
Results. The developed SOI-biosensor successfully detected target troponin I molecules at a concentration of 10–11 mol/L. The detection process exhibited an effective time of approximately 200–300 s per sample. Moreover, analysis of the detection process revealed a noticeable decrease in current within the source-drain circuit, indicative of the negatively charged complex formed by troponin I and anti-troponin I DNA-aptamer at the “liquid sample–nanowire” phase interface.
- World Health Organization. The top 10 causes of death. December 9, 2020. URL: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- Snezhitsky V.A., Yorsh I.R., Golyshko V.S., Litvinovich S.N. Infarkt miokarda: patofiziologicheskie mekhanizmy razvitiya, diagnosticheskaya strategiya i taktika lecheniya [Myocardial infarction: pathophysiological mechanisms of development, diagnostic strategy, and tactics of treatment]. Grodno: Grodnenskiy gosudarstvennyy meditsinskiy universitet; 2015; 328 p.
- Pan T.M., Wang C.W., Weng W.C., Lai C.C., Lu Y.Y., Wang C.Y., Hsieh I.C., Wen M.S. Rapid and label-free detection of the troponin in human serum by a TiN-based extended-gate field-effect transistor biosensor. Biosens Bioelectron 2022; 201: 113977, https://doi.org/10.1016/j.bios.2022.113977.
- Ojha N., Dhamoon A.S. Myocardial infarction. Treasure Island (FL): StatPearls Publishing; 2022. URL: https://europepmc.org/article/nbk/nbk537076#_article-25460_s13_.
- Gerhardt W., Nordin G., Ljungdahl L. Can troponin T replace CK MBmass as “gold standard” for acute myocardial infarction (“AMI”)? Scand J Clin Lab Invest Suppl 1999; 230: 83–89, https://doi.org/10.1080/00365519909168331.
- Morrow D.A., Cannon C.P., Jesse R.L., Newby L.K., Ravkilde J., Storrow A.B., Wu A.H.B., Christenson R.H., Apple F.S., Francis G., Tang W.; National Academy of Clinical Biochemistry. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Clin Chem 2007; 115(13): e356–e375, https://doi.org/10.1161/circulationaha.107.182882.
- Daubert M.A., Jeremias A. The utility of troponin measurement to detect myocardial infarction: review of the current findings. Vasc Health Risk Manag 2010; 6: 691–699, https://doi.org/10.2147/vhrm.s5306.
- Dhara K., Mahapatra D.R. Review on electrochemical sensing strategies for C-reactive protein and cardiac troponin I detection. Microchem J 2020; 156: 104857, https://doi.org/10.1016/j.microc.2020.104857.
- Kong T., Su R., Zhang B., Zhang Q., Cheng G. CMOS-compatible, label-free silicon-nanowire biosensors to detect cardiac troponin I for acute myocardial infarction diagnosis. Biosens Bioelectron 2012; 34(1): 267–272, https://doi.org/10.1016/j.bios.2012.02.019.
- Sharma S., Jackson P.G., Makan J. Cardiac troponins. J Clin Pathol 2004; 57(10): 1025–1026, https://doi.org/10.1136/jcp.2003.015420.
- Oliveira D.C.d.B., Costa F.H.M., da Silva J.A.F. The integration of field effect transistors to microfluidic devices. Micromachines (Basel) 2023; 14(4): 791, https://doi.org/10.3390/mi14040791.
- George Kerry R., Ukhurebor K.E., Kumari S., Maurya G.K., Patra S., Panigrahi B., Majhi S., Rout J.R., Rodriguez-Torres M.d.P., Das G., Shin H.S., Patra J.K. A comprehensive review on the applications of nano-biosensor-based approaches for non-communicable and communicable disease detection. Biomater Sci 2021; 9(10): 3576–3602, https://doi.org/10.1039/d0bm02164d.
- Tran D.P., Pham T.T.T., Wolfrum B., Offenhäusser A., Thierry B. CMOS-compatible silicon nanowire field-effect transistor biosensor: technology development toward commercialization. Materials (Basel) 2018; 11(5): 785, https://doi.org/10.3390/ma11050785.
- Kim K., Park C., Kwon D., Kim D., Meyyappan M., Jeon S., Lee J.S. Silicon nanowire biosensors for detection of cardiac troponin I (cTnI) with high sensitivity. Biosens Bioelectron 2016; 77: 695–701, https://doi.org/10.1016/j.bios.2015.10.008.
- De Moraes A.C.M., Kubota L.T. Recent trends in field-effect transistors-based immunosensors. Chemosensors 2016; 4(4): 20, https://doi.org/10.3390/chemosensors4040020.
- Generalov V.M., Naumova O.V., Fomin B.I., P’yankov S.A., Khlistun I.V., Safatov A.S., Zaitsev B.N., Zaitseva E.G., Aseev A.L. Detection of Ebola virus VP40 protein using a nanowire SOI biosensor. Optoelectron Instrum Data Process 2019; 55: 618–622, https://doi.org/10.3103/s875669901906013x.
- Patolsky F., Zheng G., Hayden O., Lakadamyali M., Zhuang X., Lieber C.M. Electrical detection of single viruses. Proc Natl Acad Sci U S A 2004; 101(39): 14017–14022, https://doi.org/10.1073/pnas.0406159101.
- Panahi A., Sadighbayan D., Forouhi S., Ghafar-Zadeh E. Recent advances of field-effect transistor technology for infectious diseases. Biosensor (Basel) 2021; 11(4): 103, https://doi.org/10.3390/bios11040103.
- Wadhera T., Kakkar D., Wadhwa G., Raj B. Recent advances and progress in development of the field effect transistor biosensor: a review. J Electron Mater 2019; 48: 7635–7646, https://doi.org/10.1007/s11664-019-07705-6.
- Sadighbayan D., Hasanzadeh M., Ghafar-Zadeh E. Biosensing based on field-effect transistors (FET): recent progress and challenges. Trends Analyt Chem 2020; 133: 116067, https://doi.org/10.1016/j.trac.2020.116067.
- Cetin Y., Aydinlik S., Gungor A., Kan T., Avsar T., Durdagi S. Review on in silico methods, high-throughput screening techniques, and cell culture based in vitro assays for SARS-CoV-2. Curr Med Chem 2020; 29(38): 5925–5948, https://doi.org/10.2174/0929867329666220627121416.
- Chiang P.L., Chou T.C., Wu T.H., Li C.C., Liao C.D., Lin J.Y., Tsai M.H., Tsai C.C., Sun C.J., Wang C.H., Fang J.M., Chen Y. T. Nanowire transistor-based ultrasensitive virus detection with reversible surface functionalization. Chem Asian J 2012; 7(9): 2073–2079, https://doi.org/10.1002/asia.201200222.
- Thriveni G., Ghosh K. Advancement and challenges of biosensing using field effect transistors. Biosensors (Basel) 2022; 12(8): 647, https://doi.org/10.3390/bios12080647.
- Bulgakova A., Berdyugin A., Naumova O., Fomin B., Pyshnyi D., Chubarov A., Dmitrienko E., Lomzov A. Solution pH effect on drain-gate characteristics of SOI FET biosensor. Electronics 2023; 12(3): 777, https://doi.org/10.3390/electronics12030777.
- Vance S.A., Sandros M.G. Zeptomole detection of C-reactive protein in serum by a nanoparticle amplified surface plasmon resonance imaging aptasensor. Sci Rep 2014; 4: 5129, https://doi.org/10.1038/srep05129.
- Yang X., Wang Y., Wang K., Wang Q., Wang P., Lin M., Chena N., Tan Y. DNA aptamer-based surface plasmon resonance sensing of human C-reactive protein. RSC Adv 2014; 4(58): 30934–30937, https://doi.org/10.1039/c4ra05011h.
- Lin M.C., Nawarak J., Chen T.Y., Tsai H.Y., Hsieh J.F., Sinchaikul S., Chen S.T. Rapid detection of natriuretic peptides by a microfluidic LabChip analyzer with DNA aptamers: application of natriuretic peptide detection. Biomicrofluidics 2009; 3(3): 34101, https://doi.org/10.1063/1.3194283.
- Pur M.R.K., Hosseini M., Faridbod F., Ganjali M.R. Highly sensitive label-free electrochemiluminescence aptasensor for early detection of myoglobin, a biomarker for myocardial infarction. Microchim Acta 2017; 184: 3529–3537, https://doi.org/10.1007/s00604-017-2385-y.
- Jo H., Her J., Lee H., Shim Y.B., Ban C. Highly sensitive amperometric detection of cardiac troponin I using sandwich aptamers and screen-printed carbon electrodes. Talanta 2017; 165: 442–448, https://doi.org/10.1016/j.talanta.2016.12.091.
- Negahdary M., Behjati-Ardakani M., Sattarahmady N., Yadegari H., Heli H. Electrochemical aptasensing of human cardiac troponin I based on an array of gold nanodumbbells — applied to early detection of myocardial infarction. Sens Actuators B Chem 2017; 252: 62–71, https://doi.org/10.1016/j.snb.2017.05.149.
- Chandola C., Kalme S., Casteleijn M.G., Urtti A., Neerathilingam M. Application of aptamers in diagnostics, drug-delivery and imaging. J Biosci 2016; 41(3): 535–561, https://doi.org/10.1007/s12038-016-9632-y.
- Squires T.M., Messinger R.J., Manalis S.R. Making it stick: convection, reaction and diffusion in surface-based biosensors. Nat Biotechnol 2008; 26(4): 417–426, https://doi.org/10.1038/nbt1388.
- Krasitskaya V.V., Goncharova N.S., Biriukov V.V., Bashmakova E.E., Kabilov M.R., Baykov I.K., Sokolov A.E., Frank L.A. The Ca2+-regulated photoprotein obelin as a tool for SELEX monitoring and DNA aptamer affinity evaluation. Photochem Photobiol 2020; 96(5): 1041–1046, https://doi.org/10.1111/php.13274.
- Stern E., Wagner R., Sigworth F.J., Breaker R., Fahmy T.M., Reed M.A. Importance of the Debye screening length on nanowire field effect transistor sensors. Nano Lett 2007; 7(11): 3405–3409, https://doi.org/10.1021/nl071792z.
- Generalov V.M., Naumova O.V., P’yankov S.A., Kolosova I.V., Safatov A.S., Zaytsev B.N., Zaytseva E.G., Buryak G.A., Cheremiskina A.A., Filatova N.A., Aseev A.L. Indication of the vaccinia virus by a nanowire silicon-on-insulator biosensor. Avtometria 2021; 57(1): 42–49, https://doi.org/10.15372/aut20210105.
- Ocaña C., del Valle M. A comparison of four protocols for the immobilization of an aptamer on graphite composite electrodes. Microchim Acta 2014; 181: 355–363, https://doi.org/10.1007/s00604-013-1126-0.
- Tan S.Y., Acquah C., Tan S.Y., Ongkudon C.M., Danquah M.K. Characterisation of charge distribution and stability of aptamer-thrombin binding interaction. Process Biochem 2017; 60: 42–51, https://doi.org/10.1016/j.procbio.2017.06.003.
- Kantor C.R., Schimmel P.R. Biophysical chemistry: part I: the conformation of biological macromolecules. 1st edition. W.H. Freeman and Company; 1980.
- Ravindranathan S., Butcher S.E., Feigon J. Adenine protonation in domain B of the hairpin ribozyme. Biochemistry 2000; 39(51): 16026–16032, https://doi.org/10.1021/bi001976r.
- Kochetkov N.K., Budovskiy E.P., Sverdlov E.D., Simukova N.K., Turchinskiy M.F., Shibaev V.N. Organicheskaya khimiya nukleinovykh kislot [Organic chemistry of nucleic acids]. Moscow: Khimiya; 1970.
- Shabarova Z.A., Bogdanov A.A. Khimiya nukleinovykh kislot i ikh komponentov [Chemistry of nucleic acids and their components]. Moscow: Khimiya; 1978; p. 584.
- Farrow T., Laumier S., Sandall I., van Zalinge H. An aptamer-functionalized Schottky-field effect transistor for the detection of proteins. Biosensors (Basel) 2022; 12(5): 347, https://doi.org/10.3390/bios12050347.
- Filatov V.L., Katrukha A.G., Bulargina T.V., Gusev N.B. Troponin: structure, properties, and mechanism of functioning. Biochemistry (Mosc) 1999; 64: 969–985.
- Serdechnyy troponin I [Cardiac troponin I]. HyTest; 2019. URL: https://hytest.ru/sites/5cd13840ff4f702c0cbc4c8d/ assets/5da43ec3fd7fb419e85444c7/ Troponin_Booklet_2019.pdf.
- Generalov V., Cheremiskina A., Glukhov A., Grabezhova V., Kruchinina M., Safatov A. Investigation of limitations in the detection of antibody+ antigen complexes using the silicon-on-insulator field-effect transistor biosensor. Sensors (Basel) 2023; 23(17): 7490, https://doi.org/10.3390/s23177490.










