Development of L1 Vertebral Anthropomorphic Model for Densitometric Phantom Improvement
The aim of the study was to develop L1 vertebral anthropomorphic model to improve the previously developed PHK FK2 phantom.
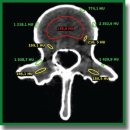
Materials and Methods. The vertebra was made using 3D printing by a digital model obtained from DICOM files of the abdominal CT examination. The phantom construction consists of three layers of different X-ray density. In the base made of photopolymer resin there is a cylindrical recess filled with a plastic mixture to imitate the normal state of the spongy substance (high density), osteopenia (moderate density decrease) and osteoporosis (significant decrease in density). Mineral density is regulated by changing β-tricalcium phosphate concentration. The cortical layer is modelled by applying metal foil on the base surface.
Results. In X-ray tube voltage of 120 kV, the mean square deviations of the measured X-ray density values of the vertebral body, spongy substance and the cortical layer were 12.40, 3.96, and 57.23 HU, respectively. The mineral density assessment of the spongy substance for three X-ray tube voltages (100, 120, 140 kV) showed the mean absolute error to be 7.4 mg/ml, and the mean relative error — 7.3% (variation coefficient). The correction coefficient equal 7 mg/ml was used to correct the values, and after using the coefficient the mean absolute error decreased up to 0.4 mg/ml, and the mean relative error — up to 0.4% (variation coefficient). The relative measurement errors of the ventral, medial and dorsal vertebral body dimensions were 3.6, 2.7, and 2.9%, respectively.
Conclusion. The methods used in developing a vertebral model can be applied in modeling the entire range of the mineral density of bone spongy substance: from osteoporosis to norm. The developed model demonstrates high stability of X-ray characteristics and anatomical accuracy; therefore, it can be used for equipment calibration, quality control of diagnostic systems, and in the training process to demonstrate the bone structure changes.
- Khoruzhaya A.N., Ahkmad E.S., Semenov D.S. The role of the quality control system for diagnostics of oncological diseases in radiomics. Digital Diagnostics 2021; 2(2): 170–184, https://doi.org/10.17816/DD60393.
- Artyukova Z.R., Petraikin A.V., Kudryavtsev N.D., Petryaykin F.A., Semenov D.S., Sharova D.E., Belaya Zh.E., Vladzimirskyy A.V., Vasilev Yu.A. Experience with artificial intelligence algorithms for the diagnosis of vertebral compression fractures based on computed tomography: from testing to practical evaluation. Digital Diagnostics 2024; 5(3): 505–518, https://doi.org/10.17816/DD624250.
- Artyukova Z.R., Kudryavtsev N.D., Petraikin A.V., Abuladze L.R., Smorchkova A.K., Akhmad E.S., Semenov D.S., Belyaev M.G., Belaya Zh.E., Vladzimirskyy A.V., Vasiliev Yu.A. Using an artificial intelligence algorithm to assess the bone mineral density of the vertebral bodies based on computed tomography data. Medical Visualization 2023; 27(2): 125–137, https://doi.org/10.24835/1607-0763-1257.
- Petraikin A.V., Belaya Zh.E., Belyaev M.G., Zakharov A.A., Bukharaev A.N., Bobrovskaya T.M., Kudryavtsev N.D., Semenov D.S., Akhmad E.S., Artyukova Z.R., Abuladze L.R., Smorchkova A.K., Vasiliev Yu.A. Accuracy of automatic diagnostics of vertebral compression fractures using data from the morphometric algorithm of artificial intelligence. Osteoporosis and Bone Diseases 2022; 25(3): 92–93, https://doi.org/10.14341/osteo13064.
- Artyukova Z.R., Kudryavtsev N.D., Abuladze L.R., Akhmad E.S., Semenov D.S. Practical application of a phantom for automated bone mineral density assessment. Osteoporosis and Bone Diseases 2022; 25(3): 10–11, https://doi.org/10.14341/osteo12974.
- Petryaikin A.V., Smolyarchuk M.Ya., Petryaikin F.A., Nizovtsova L.A., Artyukova Z.R., Sergunova K.A., Akhmad E.S., Semenov D.S., Vladzimirsky A.V., Morozov S.P. Assessment the accuracy of densitometry measurements using DMA PP2 phantom. Travmatologiya i ortopediya Rossii 2019; 25(3): 124–134, https://doi.org/10.21823/2311-2905-2019-25-3-124-134.
- Morozov S.P., Sergunova K.A., Petryaikin A.V., Semenov D.S., Petryaikin F.A., Akhmad E.S., Nizovtsova L.A., Vladzimirsky A.V. Ustroystvo fantoma dlya provedeniya ispytaniy rentgenovskikh metodov osteodensitometrii. Patent RU 186961 U1. 2018.
- Pickhardt P.J., Lee S.J., Liu J., Yao J., Lay N., Graffy P.M., Summers R.M. Population-based opportunistic osteoporosis screening: validation of a fully automated CT tool for assessing longitudinal BMD changes. Br J Radiol 2019; 92(1094): 20180726, https://doi.org/10.1259/bjr.20180726.
- The American College of Radiology. ACR–SPR–SSR practice parameter for the performance of quantitative computed tomography tQCT) bone mineral density. 2023. URL: https://gravitas.acr.org/PPTS/GetDocumentView?docId=11.
- Gromov A.I., Petraikin A.V., Kulberg N.S., Kim S.Yu., Morozov S.P., Sergunova K.A., Usanov M.S. The problem of X-ray attenuation estimation accuracy in multislice computed tomography. Medical Visualization 2016; 6: 133–142.
- Roth H.R., Wang Y., Yao J., Lu L., Burns J.E., Summers R.M. Deep convolutional networks for automated detection of posterior-element fractures on spine CT. Medical Imaging 2016: Computer-Aided Diagnosis 2016; 9785: 97850P, https://doi.org/10.1117/12.2217146.
- Kalender W.A., Felsenberg D., Genant H.K., Fischer M., Dequeker J., Reeve J. The European Spine Phantom — a tool for standardization and quality control in spinal bone mineral measurements by DXA and QCT. Eur J Radiol 1995; 20(2): 83–92, https://doi.org/10.1016/0720-048x(95)00631-y.
- Pearson D., Cawte S.A., Green D.J. A comparison of phantoms for cross-calibration of lumbar spine DXA. Osteoporos Int 2002; 13(12): 948–954, https://doi.org/10.1007/s001980200132.
- Arnold B.A., Xiang P., Budoff M.J., Mao S.S. Very small calcifications are detected and scored in the coronary arteries from small voxel MDCT images using a new automated/calibrated scoring method with statistical and patient specific plaque definitions. Int J Cardiovasc Imaging 2012; 28(5): 1193–1204, https://doi.org/10.1007/s10554-011-9914-2.
- Kweon D.C., Kim E.H., Shim D.O., Dong K.R., Kim H.S., Goo E.H., Chung W.K. Assessment of the effect of bone density and soft tissue thickness on phantom measurements. J Korean Phys Soc 2010; 5(57): 1263–1269, https://doi.org/10.3938/jkps.57.1263.
- Islamian J.P., Garoosi I., Fard K.А., Abdollahi M.R. Comparison between the MDCT and the DXA scanners in the evaluation of BMD in the lumbar spine densitometry. Egypt J Radiol Nucl Med 2016; 47(3): 961–967, https://doi.org/10.1016/j.ejrnm.2016.04.005.
- Park A.J., Choi J.H., Kang H., Park K.J., Kim H.Y., Kim S.H., Kim D.Y., Park S.H., Ha Y.C. Result of proficiency test and comparison of accuracy using a European spine phantom among the three bone densitometries. J Bone Metab 2015; 22(2): 45–49, https://doi.org/10.11005/jbm.2015.22.2.45.










